

Pulmonary arterial hypertension is a life-threatening form of right heart failure, with poor survival when treatment is delayed. Unfortunately, because PAH has vague symptoms like shortness of breath and requires invasive testing, it typically takes 2.8 years for patients to be accurately diagnosed.
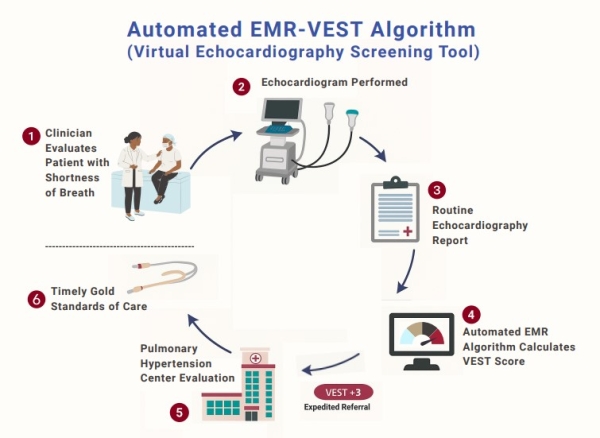
A novel screening tool closes that gap by using echocardiogram data to automatically flag patients at high risk. The virtual echocardiography screening tool, or VEST, has been shown to be highly accurate in identifying individuals likely to have PAH, said Anjali Vaidya, MD, FACC, FASE, FACP, Director of the Advanced Pulmonary Hypertension, Right Heart Failure & Chronic Thromboembolic Pulmonary Hypertension Program at Temple University Hospital, Professor of Medicine at Lewis Katz School of Medicine, who developed the algorithm.
“VEST makes early recognition of PAH possible, allowing patients to receive more timely referral for appropriate evaluation,” she said.
VEST has been integrated into Temple Health’s EMR systems, and developers are collaborating with other centers to facilitate its implementation nationally and internationally.
How VEST Works
A key value of VEST is its ability to differentiate PAH from PVH non-invasively.
The algorithm assigns each patient a score based on three standard parameters routinely captured in echocardiogram reports: left atrial size, E/e’ radio, and interventricular septal flattening.
Scores range from -3 to +3, with positive scores suggesting hemodynamics consistent with PAH, and negative scores predicting pulmonary venous hypertension. In an analysis, researchers found that a score of +3 had more than 92% specificity for PAH and an 88% positive predictive value for PAH hemodynamics.
In clinical use, the algorithm is triggered when a patient’s routine TTE shows a tricuspid regurgitation velocity (TRV) of 2.9 meters per second or higher. Patients with a VEST score of +3 are then flagged as high-risk and referred to a pulmonary hypertension center or specialist to receive right heart catheterization for a definitive hemodynamic assessment.
“This is the first time that routine interpretation of echocardiogram reports, without direct advanced review of imaging, has proven to be effective,” Dr. Vaidya said.
Closing Treatment Gaps
In a retrospective study, the team tested VEST on data from nearly 5,000 patients who had undergone TTE. They compared the algorithm with scores calculated manually and found it performed with 100% accuracy, identifying 354 patients with high-risk scores.
Concerningly, the study also found that a significant number of these patients were not receiving appropriate evaluation or care.
“Among the highest-risk patients flagged by the tool, the degree of PH was severe,” Dr. Vaidya said. “But a third had never been referred to a PH specialist.”
Of the patients referred to specialized care, nearly all received right heart catheterization that confirmed a PAH diagnosis. Of the patients who weren’t referred, few were evaluated for PAH.
“A lot of people are falling through the cracks,” Dr. Vaidya said. “Every day, patients tell me, ‘I’ve felt short of breath for years, but I’m just getting the correct diagnosis now.’”

