
A 70-year-old man with a history of ischemic cardio myopathy, ventricular tachycardia status post ablation, and prior heart failure withbiventricular ICD placement, presented to his community hospital in cardiogenic shock with an ejection fraction of 10%. Once stabilized,he was transferred to Temple for further management and high-acuity care.
Given the patient’s critical status, specialists from the Temple Heart & Vascular Institute proceeded with bioprosthetic aortic valvereplacement and six-vessel beating-heart CABG to offer the best option for a positive long-term outcome.
DIAGNOSTIC FINDINGS
- An echocardiogram revealed severe diffused hypokinesia with an ejectionfraction of 10% and severe low-grade, low-flow, low-gradient aortic stenosis,with peak pressure gradient 45mmHg.
- LV stroke volume was significantly reduced (14 ml/m2; reduced is
- Catheterization revealed under-expanded prior stenting and severemulti-vessel coronary disease.

Left heart catheterization
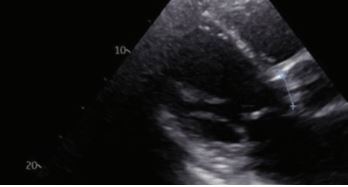
Transthoracic echo
CLINICAL COURSE
- Decided to proceed with surgery despite patient’s critically ill status.
- Patient was monitored with Swan Ganz catheter and transesophagealechocardiogram (TEE). TEE showed severe aortic stenosis and moderatemitral regurgitation at the start of procedures
- Median sternotomy revealed a mass at the upper edge of the sternum, whichwas biopsied and sent for pathology.
- LIMA was harvested in skeletonized fashion.
- Underwent high-risk bioprosthetic aortic valve replacement and six-vesselbeating-heart CABG
OUTCOMES
- At close, TEE showed well-functioning prosthetic valve and preserved LV wallmotion that was poor to start with. Cardiac output was adequate. Graft flowswere excellent.
- The patient tolerated AVR and CABG x 6 well. He was transferred to CICU instable condition.
- One week after surgery, echocardiogram showed an improved ejectionfraction of 40%.
- One month after discharge, patient demonstrated a steady recovery.
KEY POINTS
- Patients with complex cardiovascular problems and at a high risk of mortalityare often refused treatment and placed in palliative care.
- Temple offers more options for critically ill patients than any othercardiovascular surgery program in the region.
- Specialists at the Temple Heart & Vascular Institute are well known for theirhigh degree of surgical and critical care expertise, providing options whennone seemed available.
LEAD PHYSICIAN

Yoshiya Toyoda, MD, PhD
Co-Surgical Director, Temple Heart & Vascular Institute
Chief, Cardiovascular Surgery, Temple University Hospital
Surgical Director of Thoracic Transplantation,Temple University Hospital
Director, Mechanical Circulatory Support,Temple University Hospital
Professor, Surgery and William Maul Measey
Chair, Surgery, Lewis Katz School of Medicine at Temple University

